Dermal Fillers Cheek: Boost Confidence, Enhance Beauty
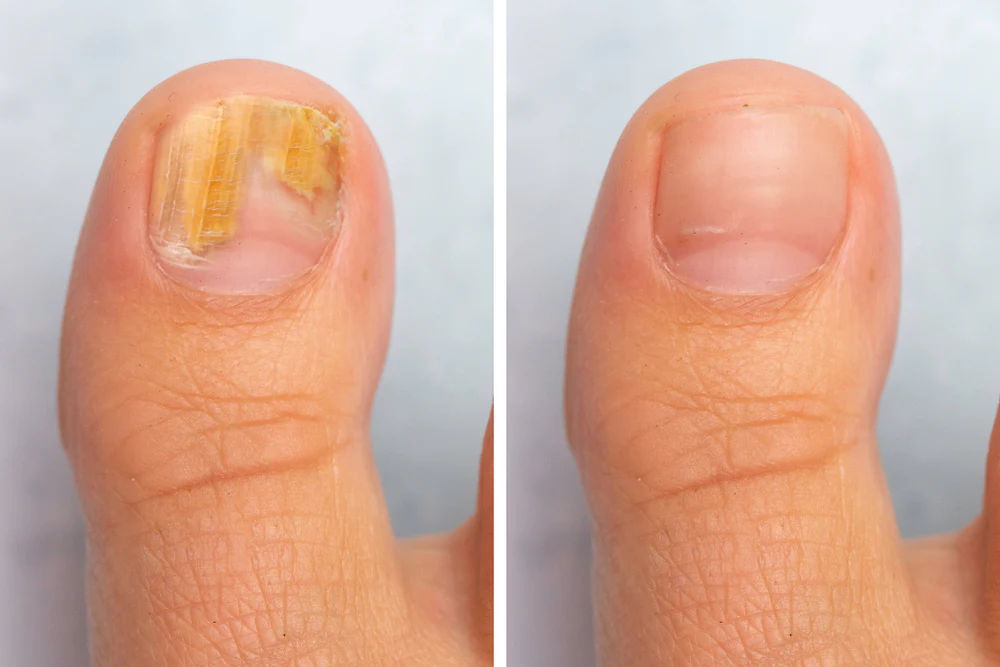
Dermal fillers are ordinarily used to work on the appearance and volume of the skin. They can reduce facial wrinkles and folds such as crow's feet and frown lines, plump up the lips and cheeks, restore lost volume to the lips and cheeks, fill in hollows under or around the eyes or nose, and smooth the area between the eyebrows vertical nasolabial folds. Do you know about the best derma fillers? Here, we will discuss the best guidelines for your needs and requirements to keep your skin bright and shiny. Filler treatments (sculpting, volumizing, liquid facelifts) are cosmetic dermatology procedures used to reduce the appearance of fine lines and wrinkles on the face and restore a more youthful appearance. It is an incredible treatment choice for those who need to take out the indications of maturing yet are hesitant to go through intrusive medicines like conventional facelifts. It fills facial areas prone to sagging to restore natural volume and fullness. While it does not provide permanent results, it offers a more accessible and safer way to look younger. Injectable dermal fillers are sensitive tissue fillers mixed into the skin at different profundities to fill facial kinks, provide facial volume, and enhance facial features. Most dermal fillers are temporary, as the body eventually absorbs them. For those who need cosmetic surgery, there is no more satisfying product and effect than the immediate correction of wrinkles or scars on the skin after injecting dermal fillers. Below are two pictures to show you the before and after comparison of patients who have injected dermal fillers. Dermal fillers can replenish lost volume and help restore a youthful appearance. They can also be used to reshape and contour the body.
Types of Dermal Fillers
The corrective fillers used to fix harmed tissues can be of various sorts. The most well-known kinds of dermal fillers incorporate.
Hyaluronic acid fillers
It is the most favored strategy, and the outcome lasts a few months to a year. Hylaform, Captique, Elevss, Juvederm, and Prevelle Silk are ordinary hyaluronic corrosive kink fillers. This kind of kink filler seldom brings about secondary effects like expansion, redness, and swelling in the infused region.
Collagen wrinkle fillers
These filters are produced using creature sources and have a higher pace of hypersensitive response. For that reason, sensitivity testing is expected before treatment begins. These infusions incorporate evolence, cosmoderm, zyplast, fibrel, zyderm and artefill.
Synthetic wrinkle fillers
This filler comprises substances arranged in the lab that are not tracked down generally in the skin. It has similar side effects to hyaluronic acid wrinkle filler but has a long-lasting effect.
Autologous wrinkle fillers
This filler eliminates fat from regions like the thighs, rump, and stomach. The fat is then infused into the face, or some other designated body part, and the impact of this filler endures for 12 to 12 years and a half. This treatment is more tedious and expensive than different techniques.
Given the patient's need, the beautician infuses a particular filler into the designated region. A few dermal fillers are available for individual use. However, intrigued competitors ought to counsel a beautician for constantly filling their facial lines. The beautician will evaluate the state of your skin and, concurringly, pick a restorative filler for facial line filling.
Temporary fillers
It can live for about six months to 2 years and decompose naturally. It is highly safe and is very popular now, such as hyaluronic acid (HA) fillers, which Thai people are very familiar with. The advantage of temporary fillers is that they can degrade and be repaired when damaged.
Semi-permanent fillers
It can last about 2-5 years, 2-5 years longer than the first filler. This type of filler is not allowed in London because the post-treatment side effects are more difficult to resolve than with temporary fillers.
Permanent fillers
There are silicone or paraffin fillers that are injected and remain in our skin layer. Doctors do not usually recommend injecting permanent fillers because they may not be completely removed if you want to remove them, which may cause long-term damage to the body.
Recovery from Dermal Fillers Cheek
You might encounter a little enlarging soon after the corrective filler's infusion. Notwithstanding, the enlarging dies down in under 48 hours. The methodology only requires up to 30 minutes, and the patient can leave the facility shortly after the treatment.
One can return to day-to-day exercises as facial line-filling margin time is right around nothing. No recuperation time is expected after dermal filler treatment, and you can return to doing everyday exercises immediately.
Facial line filler's secondary effects, such as swelling, torment, redness, expansion, tingling, and vision changes, can be avoided if specific focuses are considered. For instance, ordinary sunscreen utilization after the treatment is an unquestionable requirement. It shields the skin from future harm and forestalls post-fiery color changes.
Types of Injectable Fillers
Dermal fillers come in many types and forms and are made with different ingredients to suit different skin conditions. The most common types used by experts include:
Hyaluronic acid, or HA
These are the most common types of fillers widely used in the U.K. The main ingredient in these injectables is hyaluronic acid, a substance that some of these substances occur naturally in the body.
Hyaluronic acid fillers are versatile; doctors may recommend them to treat worry lines, crow's feet, and smile lines. The applications of these fillers aren't limited to improving skin texture, either allowing them to reshape your lips or eliminate scars.
In terms of the longevity of the results, according to a study published in NCBI.
Some well-known brands of hyaluronic acid fillers are
· Juvederm
· Preville
· Hyaluronic Acid
· Belotero Balance
Calcium Hydroxyapatite or CaHA
CaHa injectable dermal fillers resemble natural minerals found in human bone. They can add volume to cheeks, plump up nasolabial folds (deep lines running from nose to mouth), and plump up wrinkles.
Although anyone can obtain these fillers, vegans prefer them because they are a synthetic process and do not contain animal ingredients. In addition to the ethical benefits, this cosmetic filler reduces the chances of allergic reactions. CaHA fillers are believed to be safe and produce natural results. However, there needs to be more consensus that their results last only briefly; high-quality dermal fillers like Radiesse can provide results for ten to twenty months.
Polymethyl methacrylate or PMMA
If you have moderate to deep lines and wrinkles that can't be treated with HA dermal filler injections, your doctor may recommend PMMA. The results provided by these cosmetic fillers are semi-permanent, and you won't have to go back for multiple treatments as often. The most widely used PMMA brand is Bellafill, which can help you treat depressed scars, acne, nasolabial folds, and a variety of lip problems. Since the results of polymethylmethacrylate have better longevity, doctors will perform a fair number of injections to help you achieve the desired results. Some practitioners on Long Island use PMMA with "threads," a method of hiding injection marks.
Poly-L-lactic acid or PLLA
Signs of aging appear when your skin loses the ability to produce collagen. PLLA injectable filler treatment addresses this problem by naturally stimulating collagen production. The biodegradable filler dissolves in your body after a few days, but the results can last up to 24 months. Because it triggers collagen, you may need multiple injections of dermal fillers to stimulate the effects before you achieve your desired cosmetic result. Long Island's renowned practitioners often use these cosmetic fillers to treat various cosmetic disorders, such as smile lines, thin lips, and nasolabial folds. The most commonly used brand of PLLA filler is Sculptra, which is famous for its unique properties. However, the results take longer to show, but they last longer, so there is no need to repeat the injections every few months.
What is the recovery time after a cosmetic filler procedure?
Recovery time is usually short but varies from patient to patient. Full recovery requires one to two days, and you can return to your customary timetable after getting the immunization.
Many people plan their restorative filler treatment around noon and return to work quickly a short time later. Corrective fillers have fewer limitations, yet you should avoid demanding activity or perspiring until the filler has entered the skin and the swelling has died.
What are the advantages of dermal fillers cheek?
Restorative fillers are an ideal way to build up your skin, smooth out wrinkles, and reestablish the volume and average brilliance. But there are even more benefits you may need to learn about. Here are some of the unique benefits you get after receiving filler injections. While most cosmetic treatments, such as anti-wrinkle injections, can take days or weeks to work, dermal fillers can provide immediate results. While the initial results may not be dramatic, they will improve quickly to enhance your appearance. If you want to upgrade your skin for an impending occasion, restorative fillers can help you achieve the skin you want to flaunt. The risks of dermal fillers are minimal because the procedure is non-invasive. A doctor uses a needle to inject the substance into your skin to reduce scarring and pain. Patients rarely experience severe side effects after treatment, which further reduces downtime. When you choose Revitalise London Dermatology Clinic for your cosmetic filler treatment, the skilled practitioners will provide you with natural-looking facial symmetry. Contact us today for an initial consultation and to schedule your appointment. The life span of the outcomes, for the most part, relies upon the sort and brand of filler.
Nonetheless, studies have demonstrated how these outcomes can last six years and a half if appropriately kept up. When you usually pick dermal fillers to develop your skin further, you get to pick how long you believe the outcomes should endure, and the expert will suggest the filler given this. No recovery time required
If you are a regular at your favorite clinic, you can get the skin injectable procedure done in fifteen minutes. Restorative fillers are harmless, meaning no arrangement or medical procedure is required. Also, the procedure does not require you to stay in the hospital for hours; you can fit the appointment into your schedule anytime. If this is your first time going under the needle, expect slight swelling, but it will disappear within a few days.
In addition to improving the appearance of your skin, hyaluronic acid and other natural ingredients in cosmetic fillers can soften scar tissue around the injection site. If you have acne or another condition that leaves scars, dermal fillers may help. Only a board-certified practitioner can decide whether cosmetic fillers can conceal your scars. Additionally, some skin issues, such as crow's feet, are challenging to treat with fillers alone, and your doctor can use a combination approach to give you faster, longer-lasting results. Regardless of the stage of your skin condition, a medical professional can adjust the dose of filler to meet your goals. Plus, dermal fillers come in various formulas, including collagen, hyaluronic acid, and calcium hydroxyapatite, so there's a filler for almost everyone.
Risks and complications of cosmetic fillers
The non-invasive nature of dermal fillers dramatically reduces the risks and complications. However, there is a small room for risk, especially if the filler is administered by an uncertified practitioner or without assessing the patient's skin condition.
Inconveniences can go from draining to agony and expanding. These incidental effects are transitory and can be made do with non-prescription drugs.
Important Tips
If you experience any side effects after using dermal fillers, be sure to tell your doctor. Please do not take any medication without the knowledge of your medical professional, as it can affect the results.
Who Should Avoid Dermal Fillers Cheek?
Although these fillers are generally protected, they are inadmissible to everybody compared to other corrective facial infusion systems. Here are some conditions that make you a poor candidate for this procedure:
· Pregnant
· Lactation
· Autoimmune diseases
An inside and out counsel with an expert medical care professional can let you know whether you ought to go through dermal filler therapy. In addition, you can treat the underlying condition or wait until you are done breastfeeding to use fillers to enhance your beauty.
Frequently Asked Questions
Can Derma filler improve skin quality?
The Derma Filler can lift patients' skin with wrinkles, folds, or sagging.
How does beautification help?
Dermal fillers can solve many issues, including physical signs of aging and other complaints. Whether you want to fight wrinkles or add contours to your face, fillers are a great answer. Always contact a dermatologist or technician before undergoing any procedure to ensure it suits your skin.
What happened before?
Before surgery, your surgeon will schedule a consultation to assess your condition and determine your surgical goals. You should avoid taking anti-inflammatory pain medications that thin the blood, as they can build the gamble of expanding, swelling, and draining after a medical procedure. During your consultation, bring up any medications you are currently taking so we can advise you on possible conflicts.
What happens after?
When having cheek fillers in London, your specialist will utilize a skin desensitizing cream to limit torment during the technique. While patients do not usually feel pain after the procedure, some may experience slight soreness and minor bruising near the injection area. However, this is nothing to worry about, as an ice pack can reduce swelling and redness.
How do you do a derma filler appearance?
Dermal fillers can do for your appearance, particularly while battling the indications of maturing.
Common Areas for Dermal Filler Use and What to Expect
Areas of the body where dermal fillers are used include:
- Hands
- Hips
- labia majora.
- Dermal fillers can be injected under local anesthesia or sometimes without anesthesia, as some fillers contain lidocaine.
Achieve your aesthetic goals with the London Dermatology Clinic
If you're fed up with utilizing oils and salves to switch the indications of maturing, restorative fillers are an extraordinary choice. They are minimally invasive, safe, and have few side effects, making dermal fillers perfect for correcting crow's feet, deep wrinkles, and various skin concerns.
At Revitalise London Dermatology Clinic, we assess your skin condition entirely to help you understand whether fillers are appropriate for you and how they can improve your appearance. Our board-ensured specialists have long experience with injectables, and we utilize premium fillers to deliver enduring outcomes. Our Long Island facility is a truly world-class center where your vision of rejuvenated and supple skin becomes a reality.
Are you interested in cosmetic filler treatments? Visit us at Revitalise London Dermatology Clinic, 22 Harley Road, Maryleb and Westfield Mall, Stratford.
Conclusion
Ordinarily alluded to as dermal fillers, these delicate tissue fillers are substances infused into the dermis layer of the skin to reestablish the presence of barely recognizable differences and kinks while working on facial shapes. Fillers are a famous restorative system for individuals who need to work on their appearance without complex medical procedures. There are many cosmetic fillers, and their content usually depends on their intended use. Generally speaking, most dermal fillers contain hyaluronic acid, collagen, and calcium hydroxyapatite because they are safe for the skin. Unlike other methods, restorative filler medicines can be performed by a doctor in a short-term setting or at a medical spa, which reduces downtime. The procedure is relatively quick and painless. Additionally, patients can expect immediate visible results that can last for months.